Want to work smarter rather than harder? Billing in a mess? Looking for advice on how to streamline your Practice? Continue reading
Tag: genie billing
Interpret ECLIPSE Claims
TIme to decode Medicare error code 500 and 159: This example uses screen shots from the Genie Practice Management Software, but the interpretation can be applied to any ECLIPSE transaction.
It can be difficult to know which particular item is causing a multi-item ECLIPSE Claim to fail. But here is one common thing you can look for – the Medicare Codes:
Medicare codes can be confusing, so let’s look at two very common ones – Error 500 and Error 159.
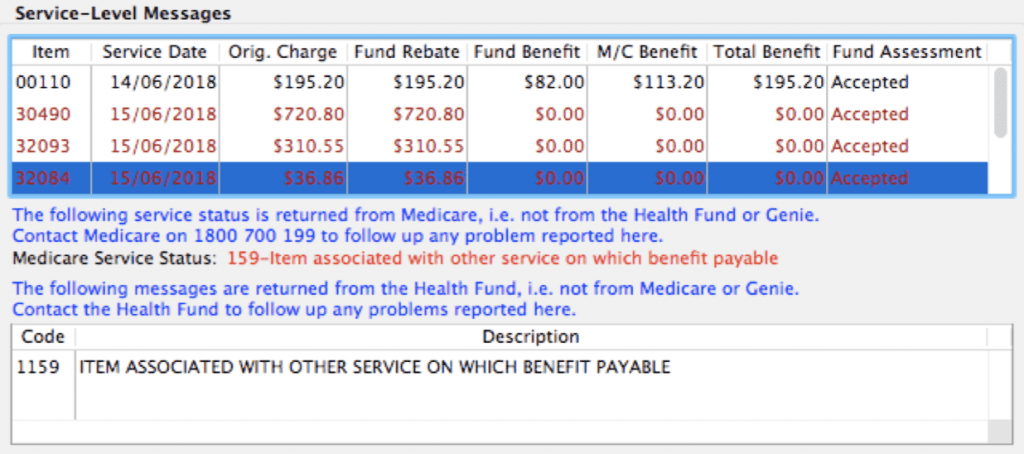
Here is a great example: This claim has three rejected items. How can we work out which one is the problem?
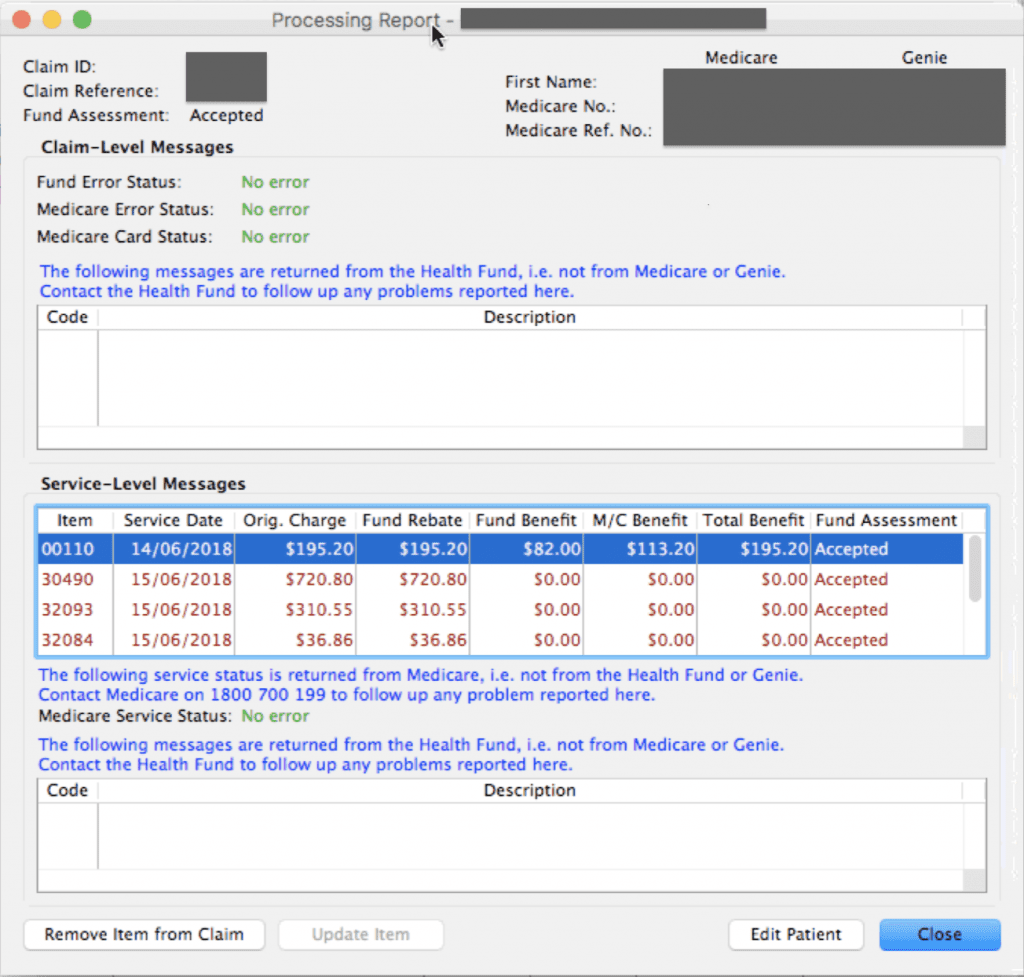
Look at the rejection message against each item. There we see:
1. ITEM 30490: This item was “rejected in association with another item”. This typically means that this item was rejected because another item in the claim has a problem, and therefore all items were rejected. Medicare will reject all items rather than guess at which might be correct. This error code usually suggests that this is not the problem item but merely rejected as a consequence of the real issue.
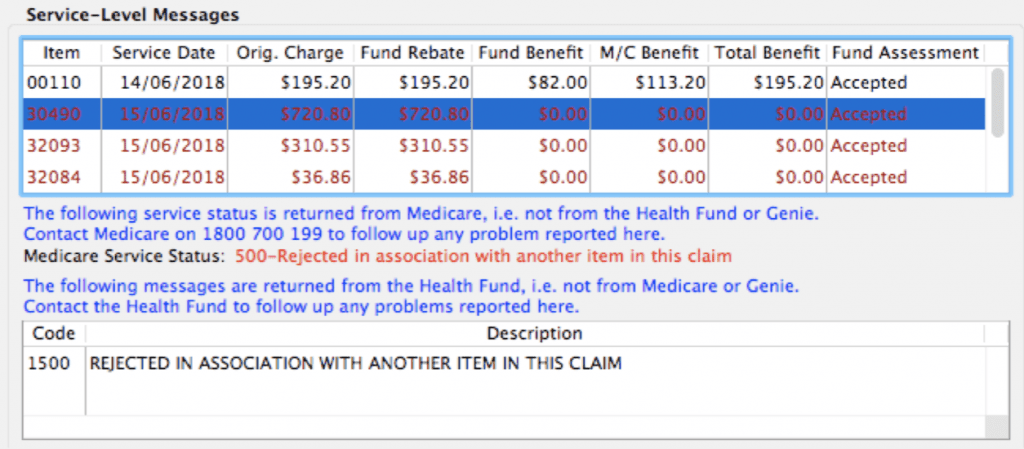
2. ITEM 32093: This next item error is the Medicare code 159 – “Item associated with other service on which benefit payable”. This typically means that this item is in conflict with another item on the claim. When we see this error, it it time to go looking for another item which may not be billed with this one.
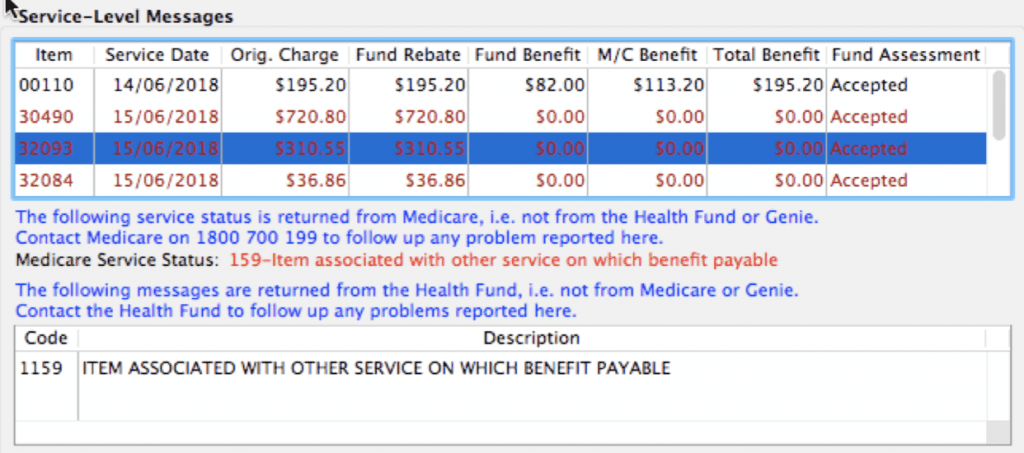
3. ITEM 32084: The third item has the same error code as the previous one – Error 159. This would indicate that this item and the one above are likely to be the culprits causing the rejection.
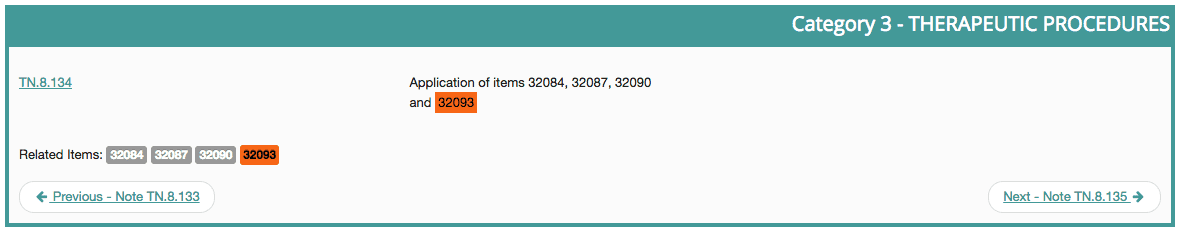
So we have narrowed the cause down to two possible items. We can check MBSOnline to investigate further. By searching MBSOnline for item 32093 we can immediately see that it is related to item 32084. Being related generally means they cannot be billed together, unless they were two entirely separate procedures, performed at different times on the same day:
As it is important not to guess with your billing, the next step is to go back to the provider, the quote or, even better, the official Operation Report, for confirmation of the correct service performed. Resubmit the correct items and credit any remaining items that were billed in error.
If in doubt – ask for help. Sometimes a little training can go a long way!
Bulk Billing Claims trick
Here is a great little trick for your bulk billing claims in Genie. Please note that this is only for FULLY REJECTED claims.
When a claim has been fully rejected, when retrieving your reports it causes a popup that says the Payment report is not available. You end up with claims that look something like this:

Part of correcting these claims typically involves removing items from the batch and deleting the exception resulting in an empty claim, or deleting the claim altogether. This is not very useful should you need to make investigations down the track. But, since I really don’t encourage you to delete anything in Genie, you do have another option that will keep the exceptions report intact, and still deal with your claim appropriately.
Whether you intend to write off the rejected items with a credit or correct and resubmit, you will remove the item/s from the claim. When you do this, my suggestion is to NOT to delete the exception when prompted. Instead, once all the items have been removed double-click the empty claim, and tick it as finalised.
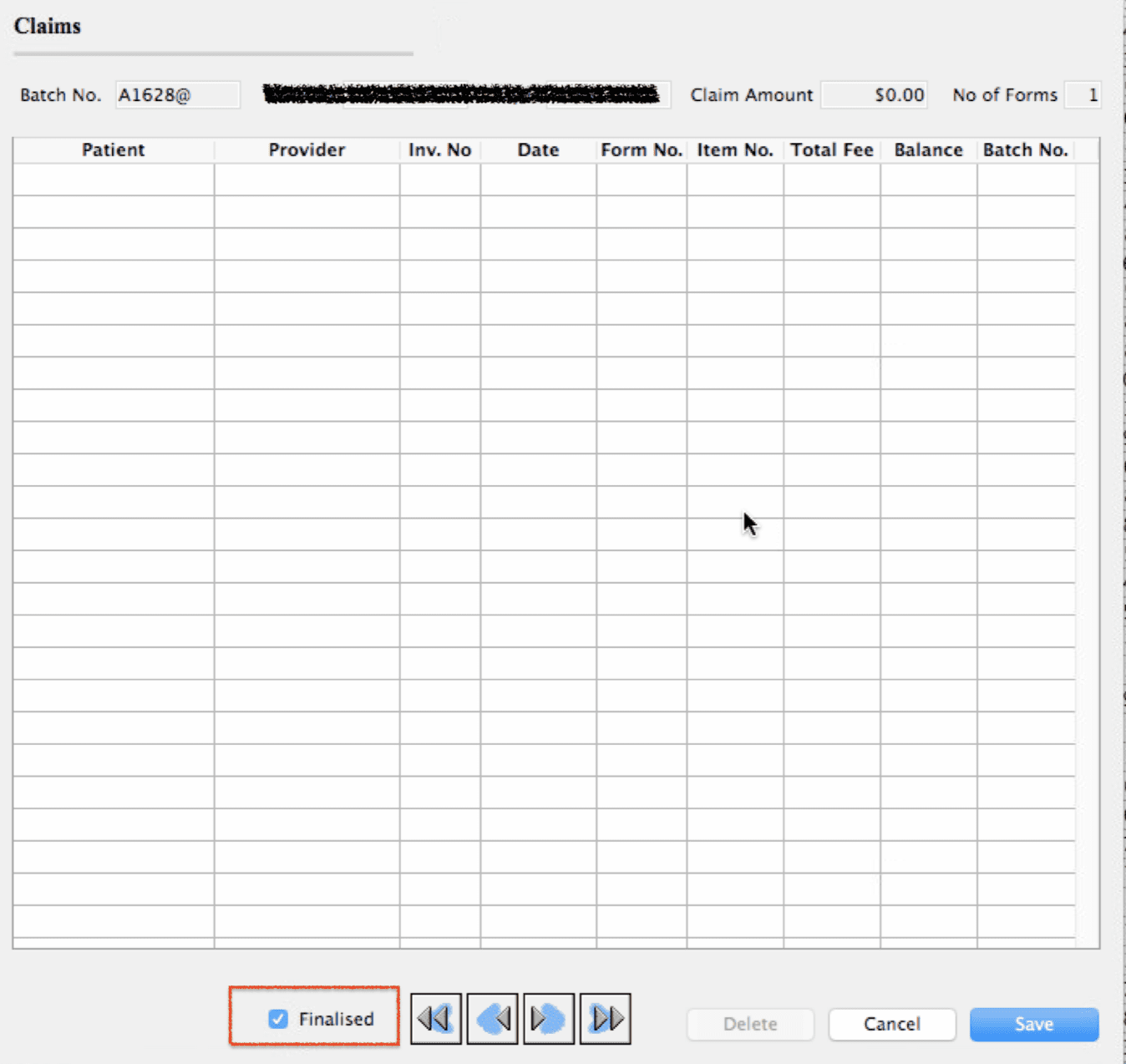
This moves it to the finalised status where the empty claim will still have full access to the Exceptions Report and the Processing and Transmission Text. This is very useful if you ever need to look back historically to see why an item was rejected.
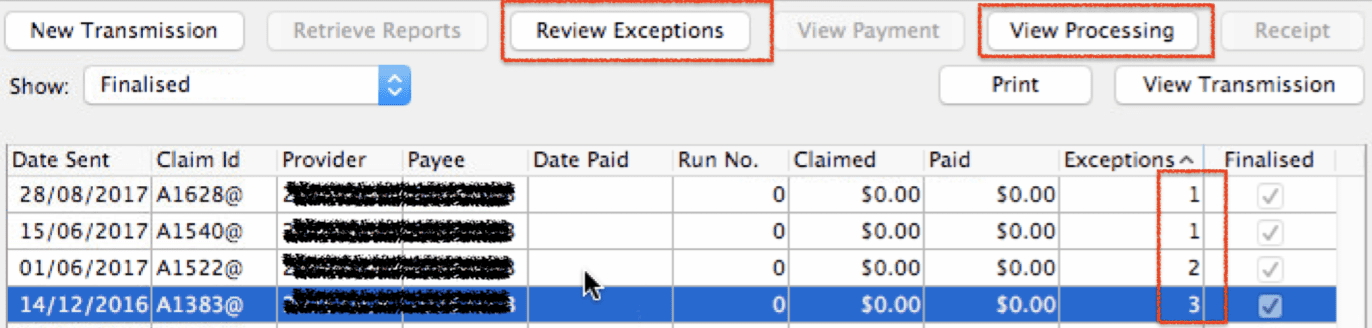
Very nice and tidy, with all the reports preserved. Give it a try!
Medicare Audits – The rules for initial consultations
Are you one of the many medical practices that have received an audit request from Medicare? You aren’t alone. Medicare has ramped up its review processes because of the many mistakes made with medical billing in both general and specialist practice.
Today I want to talk about the INITIAL CONSULT. These are typically items 104 for specialists and 110/132 for consultant physicians. The initial items in the MBS contain similar key words, Here is the 104 MBS Item description with two key phrases highlighted in red:
“Professional attendance at consulting rooms or hospital by a specialist in the practice of his or her specialty after referral of the patient to him or her—each attendance, other than a second or subsequent attendance, in a single course of treatment, other than a service to which item 106, 109 or 16401 applies”
‘Referral’ means that this service can only be supplied with the presentation of a valid referral.
A ‘single course of treatment’ is an initial attendance plus any subsequent attendances for the continuing management of the condition until the patient is referred back to the referring practitioner. That means that a new referral for the same condition does not mean you can automatically bill another initial consult item.
Another initial attendance item can be billed only if the referring doctor decides the patient’s condition needs to be reviewed and provides a new referral, and the last referral has expired, and the patient was last seen by the specialist or consultant physician more than 9 months earlier for that condition. That is a lot of ‘ands’. But, in short, it means that you cannot bill another initial consult item within 9 months of a previous visit unless the referral is for a different condition altogether.
Take a note of that: Even with a new referral, you cannot claim for another initial attendance if it has been less than 9 months since you last saw them for that same condition.
If you have received an urgent action request from Medicare to justify the 110, 132 or 104 items billed within 9 months of each other, you will need to show that they were for different conditions. If you cannot, then they need to be corrected to subsequent consult items and the monies repaid to Medicare.
If you need assistance with Medicare Audit reviews, or if you would like to get your staff billing compliantly before an audit request hits you, get in touch. We can help with review, corrective action, and training.