TIme to decode Medicare error code 500 and 159: This example uses screen shots from the Genie Practice Management Software, but the interpretation can be applied to any ECLIPSE transaction.
It can be difficult to know which particular item is causing a multi-item ECLIPSE Claim to fail. But here is one common thing you can look for – the Medicare Codes:
Medicare codes can be confusing, so let’s look at two very common ones – Error 500 and Error 159.
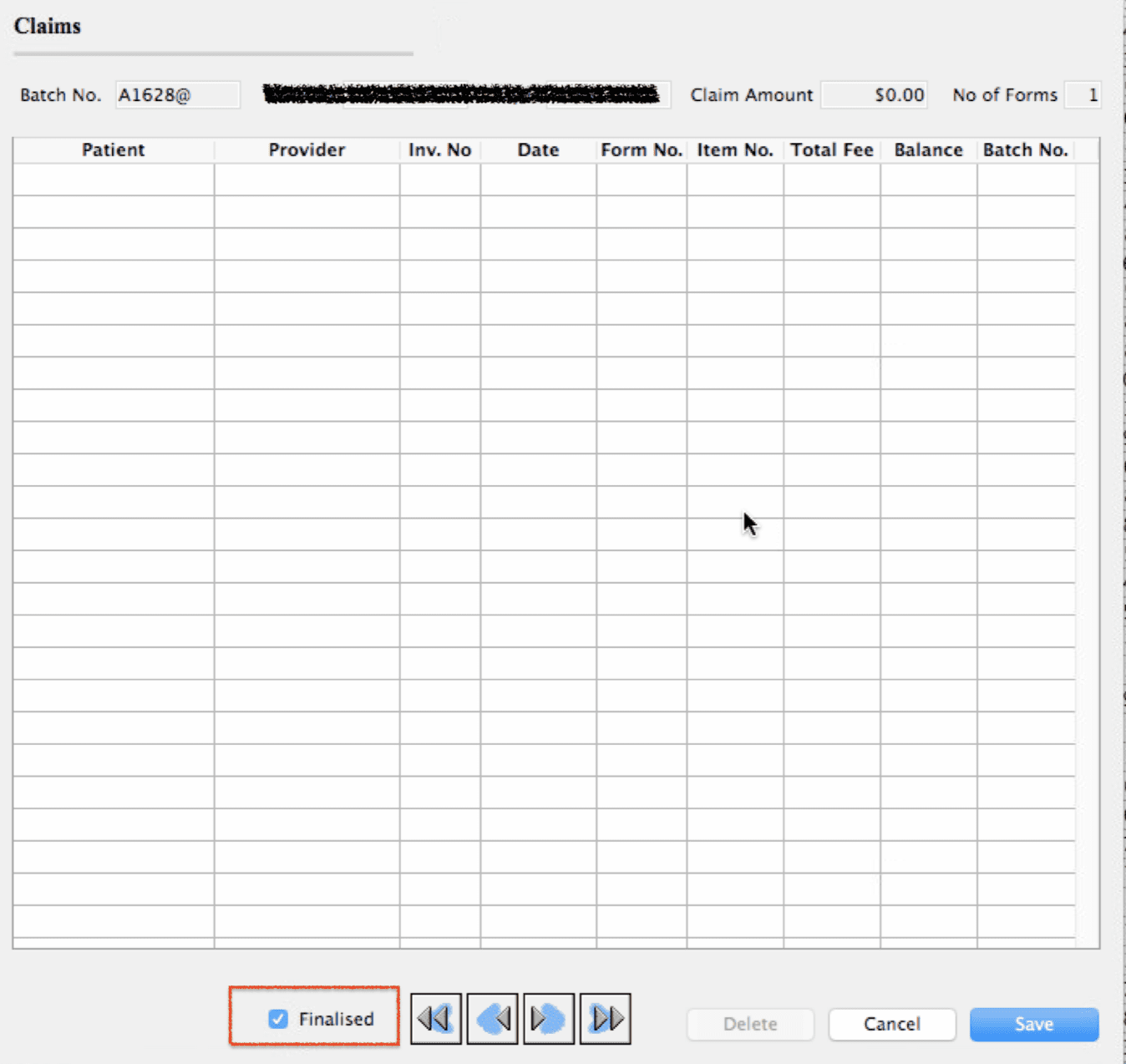
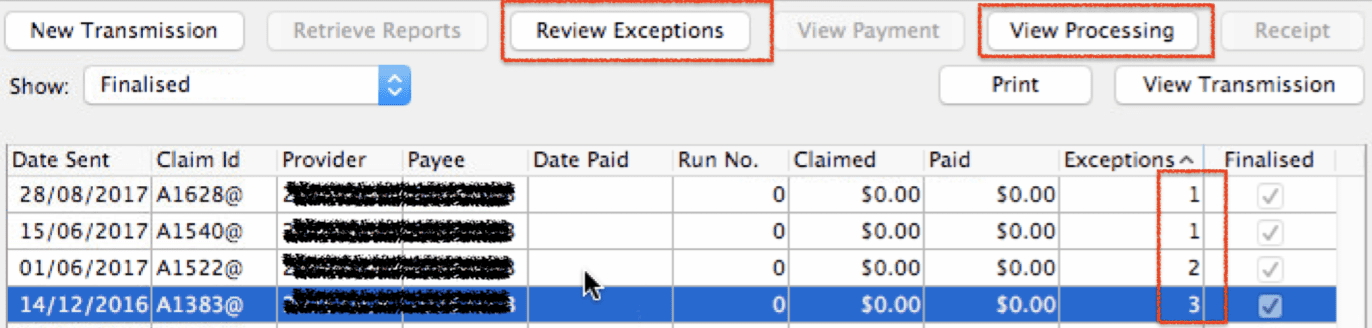
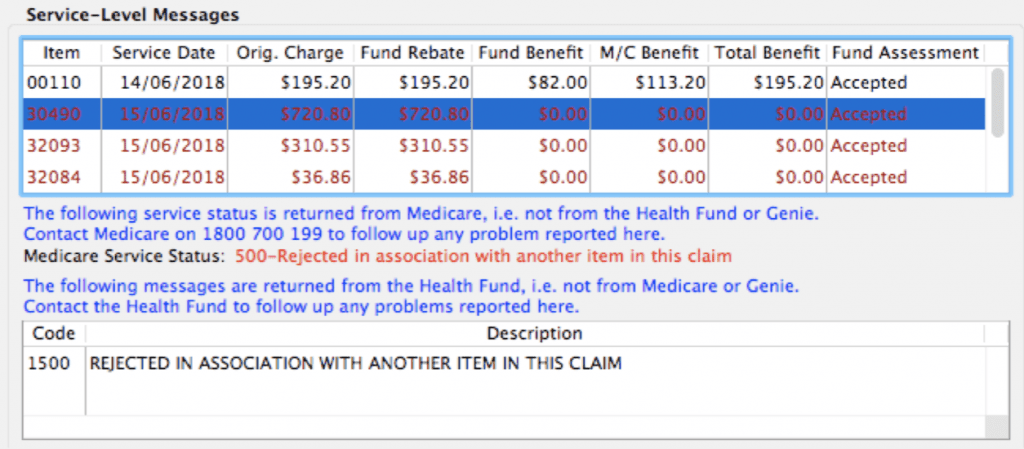
Here is a great example: This claim has three rejected items. How can we work out which one is the problem?
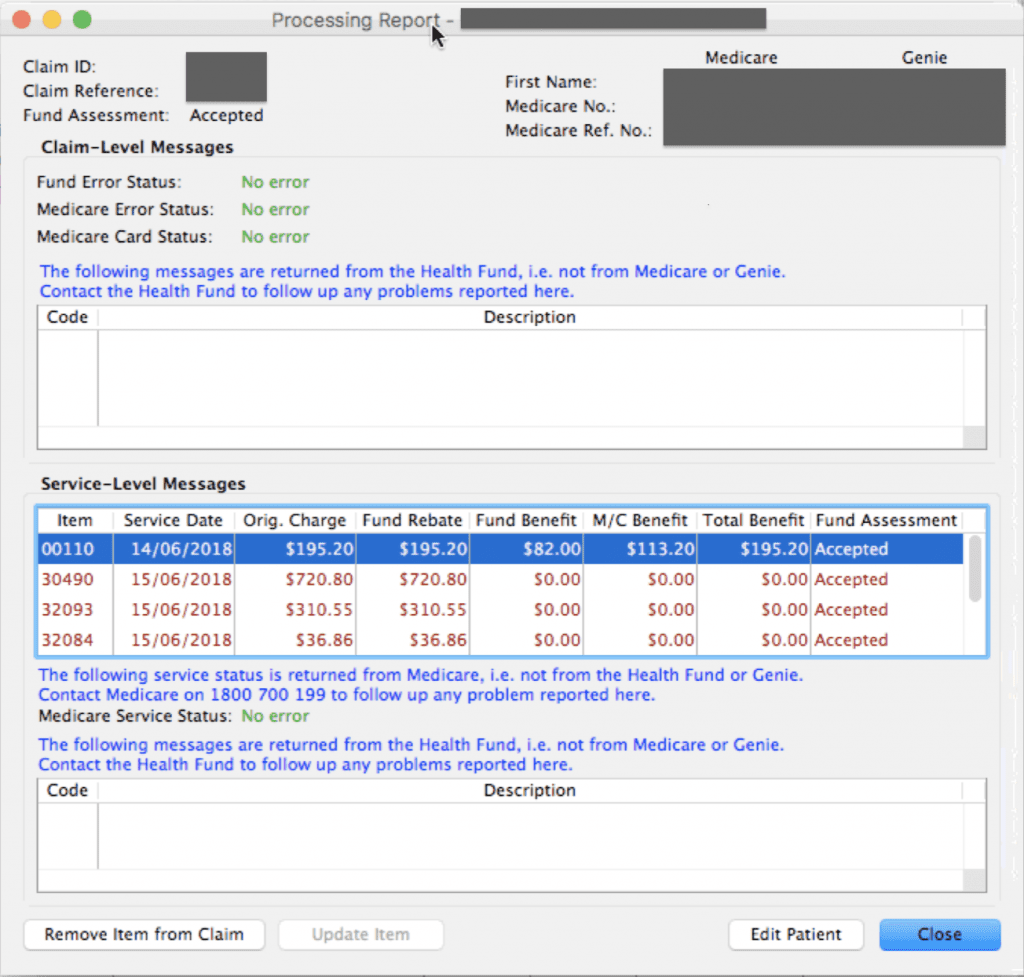
Look at the rejection message against each item. There we see:
1. ITEM 30490: This item was “rejected in association with another item”. This typically means that this item was rejected because another item in the claim has a problem, and therefore all items were rejected. Medicare will reject all items rather than guess at which might be correct. This error code usually suggests that this is not the problem item but merely rejected as a consequence of the real issue.
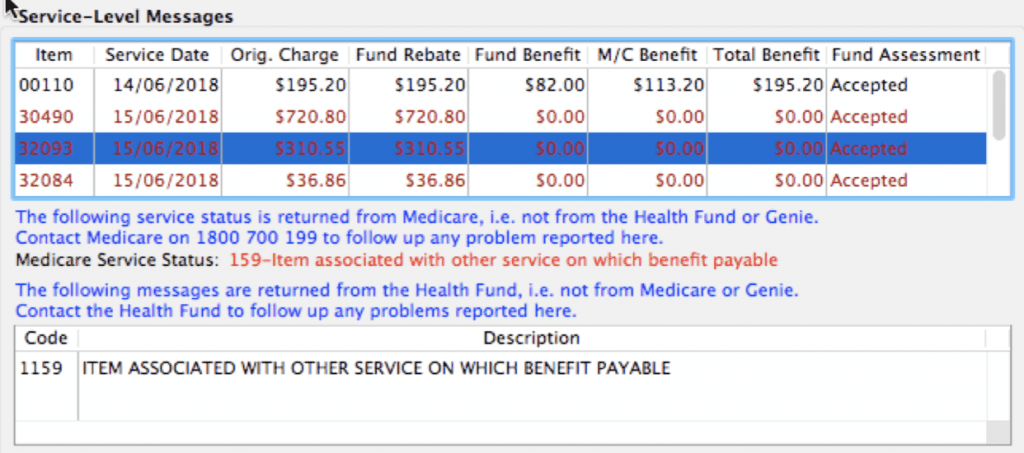
2. ITEM 32093: This next item error is the Medicare code 159 – “Item associated with other service on which benefit payable”. This typically means that this item is in conflict with another item on the claim. When we see this error, it it time to go looking for another item which may not be billed with this one.
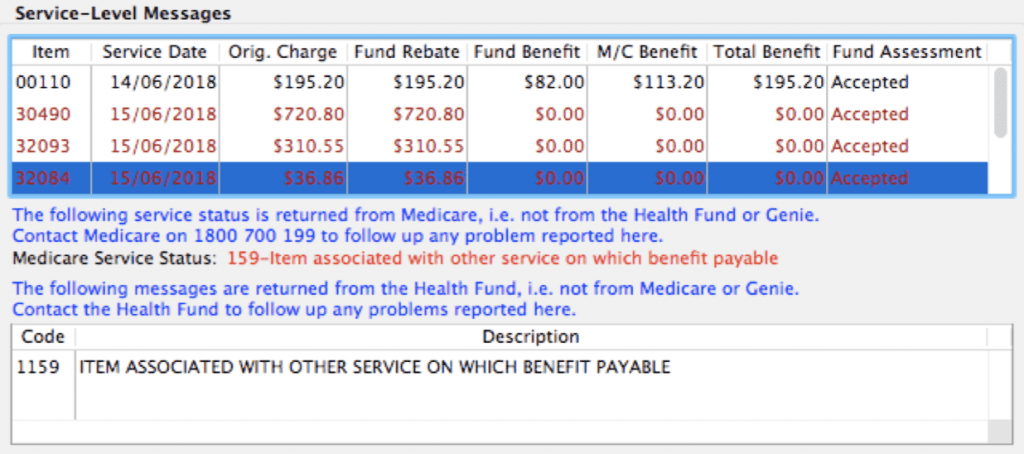
3. ITEM 32084: The third item has the same error code as the previous one – Error 159. This would indicate that this item and the one above are likely to be the culprits causing the rejection.
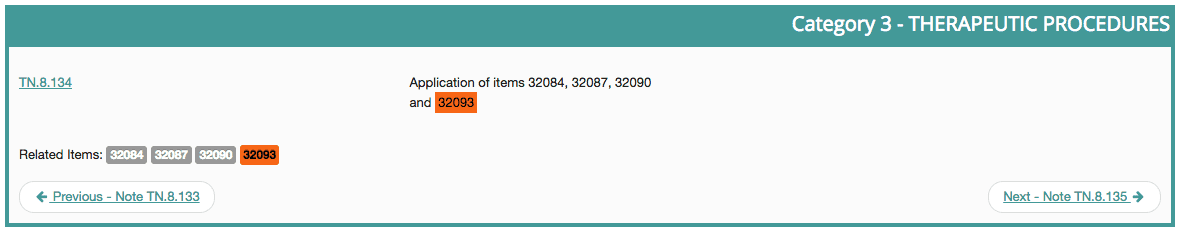
So we have narrowed the cause down to two possible items. We can check MBSOnline to investigate further. By searching MBSOnline for item 32093 we can immediately see that it is related to item 32084. Being related generally means they cannot be billed together, unless they were two entirely separate procedures, performed at different times on the same day:
As it is important not to guess with your billing, the next step is to go back to the provider, the quote or, even better, the official Operation Report, for confirmation of the correct service performed. Resubmit the correct items and credit any remaining items that were billed in error.
If in doubt – ask for help. Sometimes a little training can go a long way!